Prostate biopsy

|
|
|
|
|
||||||||||
|
|
|
|
|
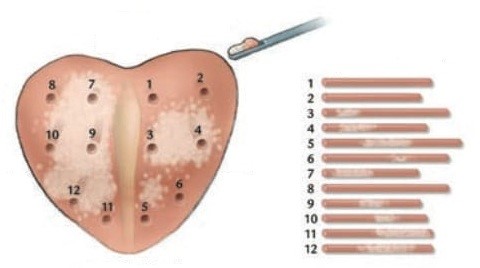
At the end of the examination, a gauze impregnated with local anesthetic and antiseptics is inserted into the rectum. The obtained tissue pieces from each area of the prostate are immediately placed separately in different vials with formalin solution and sent to the pathology laboratory for histological examination. The majority of examinees do not present any serious complication or disorder. Prophylactic antibiotics following the instructions given by the urologist helps to avoid possible infection. Blood in the urine may appear after the procedure, however after some hours and after a few emptyings of the bladder, it disappears. Rarely and in very serious cases, it is deemed necessary to insert a catheter to carry out washings. In patients with benign prostatic hyperplasia, urinary retention is likely to occur and catheter placement may be required.
|
|
||||||||||
|
What should you watch out for after the biopsy? • Your urine may be pink or rarely red, or you may even urinate small clots of blood after the test or when straining during a bowel movement. This is normal. The presence of blood in the urine will stop on the same day or after two to three days. Contact your urologist immediately if you have: |