Male Infertility

General information
Infertility is defined as the inability of a couple to achieve conception and have a child after at least one year of regular sexual contact without contraceptive protection. According to the definition of health, as formulated by the World Health Organization (WHO), infertility is a health disorder that needs treatment.
Procreation and the creation of a family are considered the right of every human being.
|
|
|
It is important to emphasize that the term infertility applies equally to men and women. As for the causes, in 40% the male factor is involved, in 40% the female factor and in the remaining 20% both are "responsible". It is divided into primary, when the couple has not had a previous pregnancy, and secondary, when one of the two partners has had a child in the past.
|
|
||||||||||
|
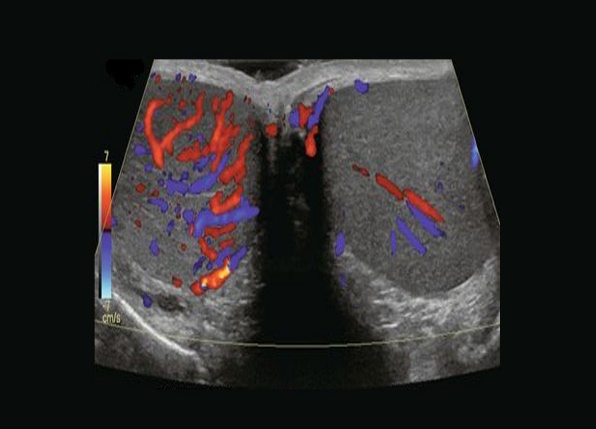
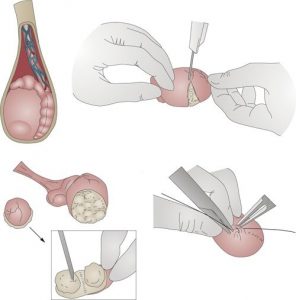
During the clinical examination, the doctor will check the penis, the scrotum, in which the testicles are located, the epididymis and the vas deferens, which is the passageway for sperm from the testicles and epididymis to the urethra. Finally, secondary sexual characteristics, such as hair growth, muscle mass and voice timbre, will also be examined. In summary, the clinical examination should include: A key tool in controlling a man's fertility is the sperm chart. It must be performed in specialized centers and its main characteristics are sperm volume, sperm concentration per ml of semen, total sperm count and sperm motility. • It is important to emphasize that there are no clear boundaries between "normal" and "pathological" spermogram. Thus, the World Health Organization has delineated some reference values, which when not met in a sperm chart, the man has reduced chances of achieving conception in the normal way. In general, semen should have: When spermatozoa are not found in the semen analysis, then we speak of azoospermia. Causes of azoospermia are obstructive or non-obstructive. In obstructive azoospermia, sperm produced at normal rates in the testicles are unable to exit the urethra due to obstruction of the ejaculatory duct of the sperm (e.g., inflammation) or due to a genetic abnormality. Measurement of sperm DNA fragmentation (DFI, DNA Fragmentation Index) In the context of prevention, but mainly treatment, the urologist is called upon to offer modern surgical solutions such as: These operations today can and should be performed with the help of microsurgery and the use of sophisticated surgical microscopes that achieve the maximization of the special skills required by the urologist specialized in microsurgery.
|
Infertility

Infertility is defined as the inability of a sexually active couple to achieve pregnancy during one year of free and regular (2-3 weekly) sexual intercourse.
Today about 30% of couples do not achieve pregnancy within a year, of which 15% undergo infertility testing and less than 5% ultimately remain childless.
|
|
|
What are the main causes of male infertility? The smoking habit is known to increase the possibility of heart and vascular problems (coronary heart disease, myocardial infarction, narrowing of large and small vessels of the body, such as the carotid and iliac arteries). However, it seems that its role is also important in fertility problems for both men and women. So there are studies that prove that the possibility of erectile dysfunction and complications during pregnancy is greater for smokers. In male smokers, a reduced number of spermatozoa (oligospermia), reduced motility (asthenospermia) and an increased number of shape abnormalities (teratospermia) are often found in the sperm count. Smoking appears to reduce the sperm's ability to fertilize the egg. |
|
||||||||||
|
|
|
|
|
Genetic assessment - karyotype A significant number of male fertility disorders, also described as idiopathic male infertility, are essentially genetic in origin. |
|
||||||||||
|
Empirical treatments We often prescribe empirical treatments, such as the administration of vitamin E, tamoxifen, or complexes of vitamins and antioxidant agents. There is no strong literature, but some men with idiopathic oligoasthenospermia will benefit. Surgical treatment Specialized microsurgical procedures |