|
How can the disease progress?
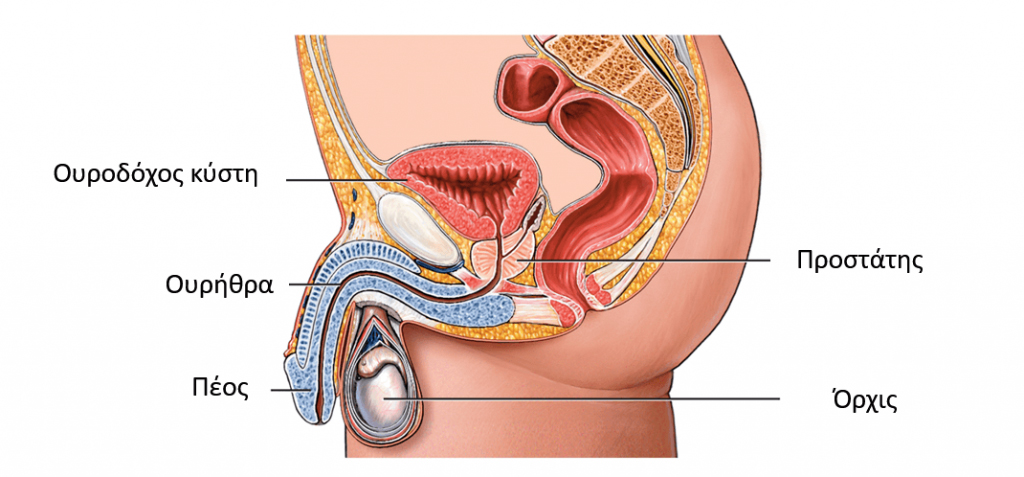
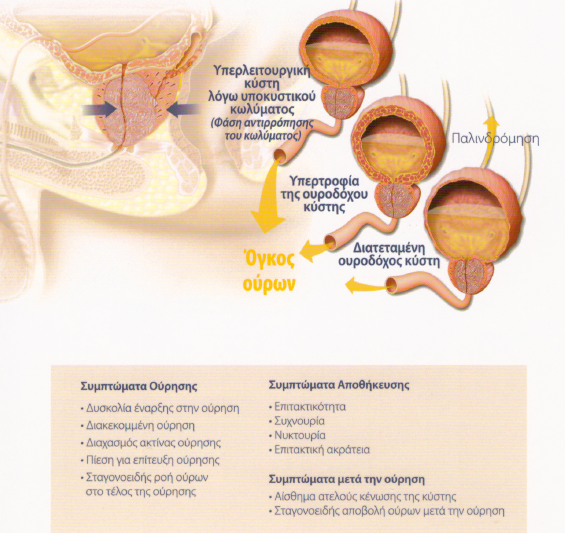
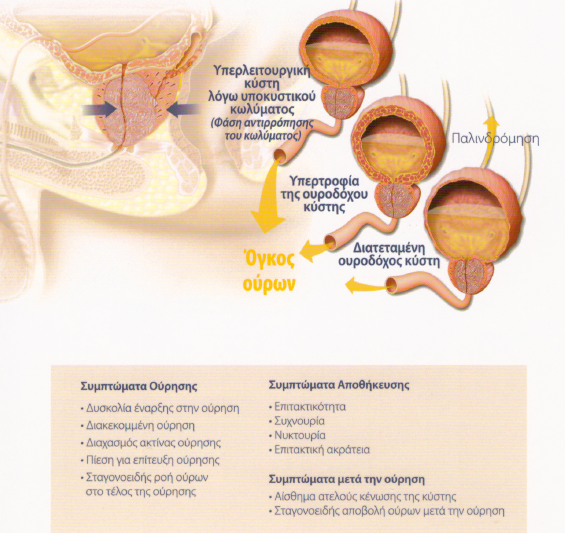
In fact, the prostate grows, but the bladder suffers, since its responsibility is both the storage of urine and its elimination, i.e. urination. So, to be able to overcome the prostate barrier, the bladder muscle is overfed, to exert more pressure on the urine, so that it overcomes the blockage.
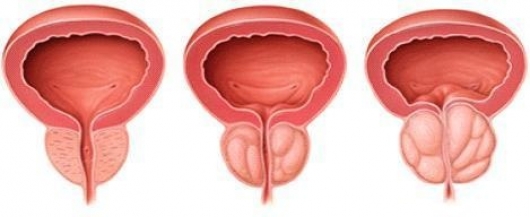
In general, we talk about medium glands when they are over 40 grams and large ones over 80 grams. Of course, this is not absolute, since the effect on urination is also determined by its composition. Thus, a small gland of 30 grams can even cause urinary retention, whereas a prostate even over 100 grams can cause mild or moderate symptoms. Also, the presence of a medial lobe projecting into the bladder is usually a significant problem since it further obstructs the flow of urine.
The hypertrophy of the bladder cannot, however, continue indefinitely. Due to the chronically increased pressures, the bladder gradually loses its elasticity and thus from a certain point a quantity of urine remains after urination, the so-called residual urine. A residual urine of more than 100ml is considered pathological, since it shows that the bladder is not contracting sufficiently. Also, stagnant urine can become infected, resulting in UTIs. The existence of residual urine is also a predisposing factor for the formation of stones in the bladder. Gallstones can cause pain and often hematuria.
Slowly, the remnant increases and the thickness of the cyst wall decreases and passively the cyst stretches. Thus, the residual can reach 2 to 3 liters. In such neglected conditions, the urine produced in the kidneys cannot go down into the bladder, the kidney calyxes stretch and lose their shape – that is, the so-called hydronephrosis occurs. If the obstruction persists and a catheter is not immediately placed, the parenchyma of the kidney is destroyed, and the patient develops renal failure.
|
|
|
Diagnosis of the condition
Diagnosis will begin with taking a medical history. The type of discomfort, how severe it is, the time of its appearance and its frequency are key elements that will be asked by your doctor. For a better picture of the problem, your doctor will ask you to fill in a special questionnaire (International Prostate Symptom Questionnaire-IPSS). This is followed by the clinical examination which includes the digital examination of the prostate. It is a basic examination, since it gives the first information on the size of the gland, its constitution and possible suspicion of hardness in the constitution of the prostate, a point suspected of coexisting malignancy.
The basic examination is the measurement of urine flow, i.e. uroflow. The patient urinates inside a special machine that measures the flow, the amount of urine excreted and the time of urination. Usually the test is completed with an ultrasound of the kidneys, ureters, bladder and prostate as well as with an assessment of the residual urine, i.e. the amount of urine that remains in the bladder after urination.
During the first visit, the doctor may ask you for a general and urine culture, as well as some blood tests, such as urea and creatinine, to check kidney function. You will also usually be asked to have a prostate specific antigen (PSA) test.
In some cases, an endoscopic examination, cystoscopy, is performed, where, with a special flexible tool with a small camera on the end, we observe the urethra, prostate and bladder with direct vision.
Finally, in special cases, an additional imaging test is used, the CT scan of the upper and lower abdomen, as well as the urodynamic test, a special test that studies the function of the bladder and urethra. The purpose of all examinations is for the doctor to distinguish the effects of the condition, so that he can determine the correct therapeutic strategy in collaboration with the patient.
Treatment of prostatic hyperplasia
Today, there are many treatment options, capable of solving every man's problem. Your urologist will recommend the most suitable ones for you and help you decide which one to follow. The decision is always made on an individual basis based on the man's history, test findings and wishes.
-Active monitoring.
This is recommended for patients with mild symptoms, which do not have significant effects on their daily life. This treatment option includes changes in the patient's lifestyle, dietary changes, fluid control and restriction before going to bed at night, urinating before going to bed, avoiding coffee and alcohol that have a diuretic and irritating effect, treating constipation, controlling medicines that the patient uses for other conditions and possibly worsen the symptoms. A large proportion of men on active surveillance will not need additional treatment for 5 years.
Medication
Recommended for men with moderate or severe symptoms. Traditionally there are two major classes of drugs, α-blockers and 5α-reductase inhibitors. Additionally and depending on the symptoms, we also use antimuscarinic drugs, phosphodiesterase inhibitors, phytotherapy as well as combination treatments.
We usually start treatment with an α-blocker. There are several formulations in this class with similar efficacy and a similar side effect profile. The ones mainly available in Greece are alfuzosin, tamsulosin and silodosin. These drugs interfere with the dynamic element of the obstruction, causing a breakdown of the smooth muscle fibers of the prostate and the bladder neck without affecting the size of the prostate. They are safe drugs and will provide symptom improvement in two-thirds of our patients. These drugs can cause mild hypotension and for this reason we usually advise taking them at night before going to bed. Another possible side effect is the reduction or elimination of sperm, without affecting the hardness of the erection or the orgasm. This is due to a quantity of sperm returning to the bladder due to a breakdown of the internal sphincter. This is called retrograde ejaculation and is restored after stopping the drug.
The second class of drugs are the 5α reductase inhibitors (finasteride and dutasteride). They are drugs that reduce the size of the prostate by about 25-30% within a period of 6 months. We usually recommend them to men with larger prostates over 50 grams with moderate or severe symptoms. 5α-reductase inhibitors are the only drugs that reduce the likelihood of urinary retention, need for future surgery, and progression of benign hyperplasia. However, like all drugs, they can have side effects and the main one that can be observed in 20% of men is the reduction of sexual desire.
In men with moderate or severe symptoms and large prostates, a common contemporary option is combination therapy with an α-blocker and a 5α-reductase inhibitor. There is even a formulation available, i.e. in one capsule there are both components. The reception takes place in the evening. Combination therapy is a safe and effective option with an optimal result, but it can cumulatively accumulate the side effects of both drugs. The doctor will discuss all this with the man and the treatment decision will be made individually, depending on the wishes and expectations of the patient.
Anticholinergics alone or in combination with an α-blocker may be tried in men with predominant symptoms of overactive bladder, ie, urgency, frequency, nocturia, and urge incontinence. In these men, of course, the possibility of something else being hidden behind these symptoms, such as bladder cancer and lithiasis, must first be ruled out. Antimuscarinics act on the bladder causing damage to its wall. They are generally safe drugs and the most common side effects they may experience are constipation and dry mouth.
Phosphodiesterase inhibitors are excellent drugs for erectile dysfunction. In the last decade, large published studies have shown that in addition to improving erections, they can also improve symptoms from the lower urinary tract due to benign prostatic hyperplasia. Today, tadalafil is commercially available at a low dose of 5 mg for daily administration. It is a very good choice for men who have both symptoms of benign hyperplasia and erectile dysfunction. The problem in Greece is that it is not prescribed through the funds and the man pays the full cost of the medicine.
Phytotherapy is a common choice in men with benign hyperplasia that causes mild symptoms and is steadily gaining ground in the treatment of BPH. The problem is that there are no large randomized studies that give clear results. The exact mechanism of action of phytotherapy is not clear. In the laboratory they appear to have anti-inflammatory and anti-androgenic properties, but this has not been sufficiently confirmed in humans. In general, however, great care is needed with preparations sold over the internet. Always consult your doctor!
Whatever medication is chosen, it is extremely important to monitor the man over time with a specific monitoring program determined according to the therapeutic effect.
Surgical treatment
Surgical treatment is indicated when, despite medication, the patient's symptoms persist and significantly affect the quality of his life, or when we have complications related to the K.Y.P.
The absolute indications for surgical treatment of BPH are urinary retention, renal failure due to obstruction, recurrent hematuria due to BPH, cystitis, bladder diverticulum, and recurrent UTIs. Large and worsening residual urine may also be an indication for surgical intervention.
Today, the most frequent indication for surgical treatment is the relief of "annoying" lower urinary tract symptoms due to BPH that are resistant to drug therapy.
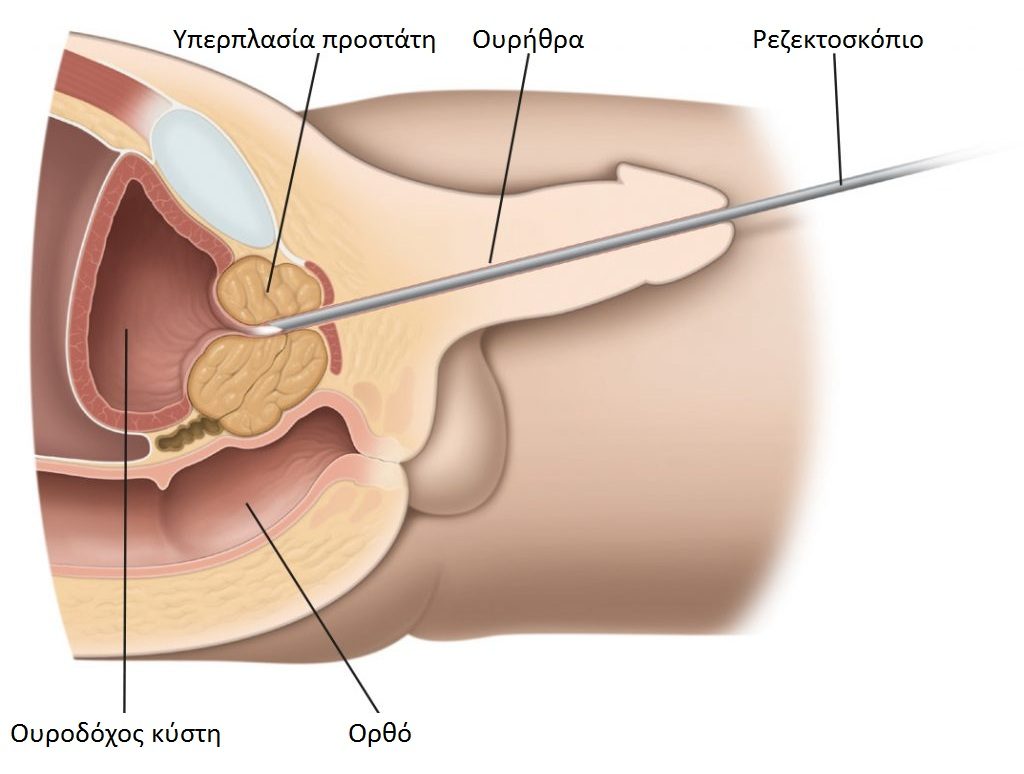
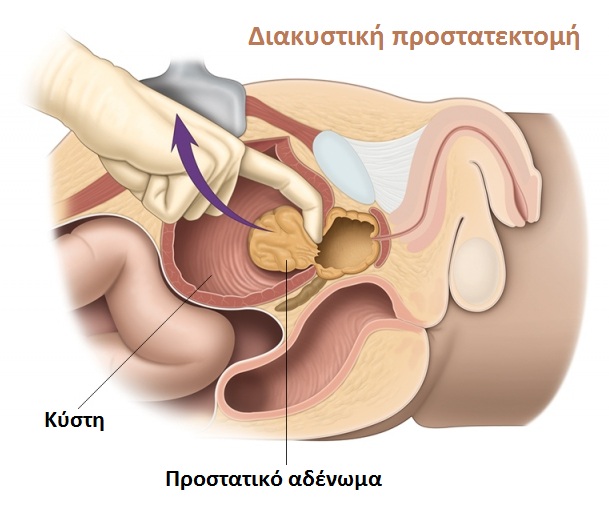
Classic (unipolar) Transurethral Resection of the Prostate (TUR-P, Transurethral Resection of the Prostate)
It is an endoscopic operation, in which the obstructing part of the prostate gland is removed through the urethra. With endoscopic techniques it is possible today to achieve the same surgical results as in the past with open surgical techniques, while at the same time operations through the urethra are less traumatic and with significantly lower rates of complications and side effects. After surgery, symptoms improve in 70–90% of patients. IPSS score decreases by approximately 85% and peak urine flow increases by 8–18ml/sec. The most common complication is retrograde ejaculation.
|